



Context - Biocides are added to many consumer goods such as cosmetics and detergents to kill bacteria or inhibit their growth. They include disinfectants, preservatives as well as antiseptics and are widely used in animal husbandry, food production and health care.
There is concern that this widespread use of biocides may lead to the emergence or proliferation of harmful bacteria that are resistant to both biocides and antibiotics.
In the light of current scientific evidence, can biocides lead to antibiotic resistant bacteria?
An assessment by the European Commission Scientific Committee on Emerging and Newly Identified Health Risks (SCENIHR).
The answers to these questions are a faithful summary of the scientific opinion produced in 2009 by the Scientific Committee on Emerging and Newly Identified
Health Risks (SCENIHR): "![]()
1.1 Bacteria can be killed or inhibited by different antimicrobial products, namely antibiotics that act against infections in humans or animals and biocides such as disinfectants and preservatives. Only products that act against bacteria are the focus of this assessment and not biocides used to control other micro-organisms or plants and animals. More...
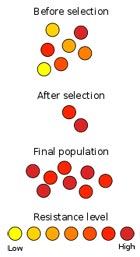
1.2 Some bacteria are naturally unaffected by antimicrobial products, and others may develop resistance to certain biocides over time. Resistant strains of bacteria can survive biocide concentrations that would kill most bacteria of the same species. Bacteria can become increasingly tolerant to antimicrobial substances so that they can withstand progressively higher concentrations. In some cases, resistance against biocides can lead to resistance to antibiotics. More...
1.3 There are many biocidal substances on the market that act in different ways and sometimes different biocides are combined in a product to increase the overall effectiveness. More...
1.4 Biocides need to be approved before they are released on the market. However, unlike antibiotics for which the use in humans and animals is carefully monitored, biocides can be used without any kind of monitoring. The total quantities of biocides produced and used in the EU remain unknown, although they are expected to be considerably greater than the total production of antibiotics.
The fact that biocides are used extensively in many different products and in huge volumes could contribute to bacteria becoming resistant to both biocides and antibiotics. More...
2.1 In health facilities, biocides are indispensable to prevent and control infections.

2.2 Biocides are added to many consumer goods to prevent micro-organisms from growing on them and spoiling them. They are included in cosmetics and personal care products, cleaning products, laundry detergents, and disinfectants. More...
2.3 In the food industry, biocides are widely used to disinfect the facilities and any equipment that comes into contact with food, as well as to decontaminate animal carcasses. They are also added as preservatives to food products, and as disinfectants to drinking water. More...

2.4 When breeding and raising livestock, the animals themselves, their products and any housing and equipment used are usually treated with biocides to decontaminate them, prevent the growth of potentially harmful micro-organisms and protect the animals from diseases. More...
2.5 Water treatment plants add biocides to the treated water before it leaves the waterworks to avoid releasing harmful organisms into the environment. Other growing industrial applications of biocides include intensive use in cooling towers to prevent the spread of Legionella carried by tiny water droplets, and the addition to building materials or to the surfaces of products to stop micro-organisms from growing on them. More...
3.1 A common way of determining resistance to biocides is to measure the minimum concentration of a biocide that will stop the growth of micro-organisms. However, a better measure of resistance is the minimum concentration needed to kill the micro-organisms. An increase in the amount of biocide needed indicates that the micro-organisms are becoming resistant to it More...
3.2 Bacteria resistant to the active biocidal substances used in health care settings have long been observed, for instance bacteria resistant to antibiotics or to the silver compounds included in compresses applied to burn wounds. Because of the widespread use of disinfectants and antiseptics in health care settings, further research is needed, not only in the laboratory but also in practice, to see if their long-term use has an effect on the emergence of resistance. More...
3.3 Bacteria resistant to biocides have been found in cosmetics and other consumer products and in the industrial plants that manufacture them. However, to date there is no direct evidence of a link with antibiotic resistance. More...
3.4 Biocides are used widely in food production and there is evidence that some harmful bacteria found in food are becoming increasingly tolerant to biocides, although they are not yet resistant to them. There is a lot of research on whether using antibiotics in animals leads to the emergence of resistant microbes. However, data on the role that current cleaning and disinfection regimes in food production and in animal husbandry may have on the emergence of resistance are scarce. More...

3.5 Because biocides are used in large volumes and discharged with wastewater, they are present at low concentration throughout the environment. There is concern that this could lead to the selective survival of resistant bacteria. More...
4.1 Some bacteria are naturally unaffected by antimicrobial products. Other bacteria find ways to keep their inside concentration of biocides at levels that are harmless to them, for instance by limiting the amount that penetrates the cell or by pumping biocides out. Some bacteria can use enzymes to alter antimicrobial products or can modify their external envelope so that products cannot penetrate inside the cell.
Of particular concern are bacteria that become resistant because they acquire resistance genes from other bacteria. More...
4.2 Bacteria can become resistant to antibiotics as a result of spontaneous changes in their DNA (mutations) or a gene transfer from another bacterium.
When different strains of bacteria are exposed to antibiotics, those that have resistance genes survive while the others are killed. Over time, this can lead to the selective survival of resistant strains, and to an increase of resistance.
Bacteria that are resistant to several classes of antibiotics at the same time (multi-drug resistant) are often found in hospitals and are a serious cause for concern. More...
4.3 Antibiotics and biocides sometimes work in similar ways and different mechanisms have enabled some bacteria to become resistant to both. This raises concerns over the indiscriminate and often inappropriate use of biocides in situations where they are unnecessary, because it can contribute to the development and persistence of resistance. More...
The possibility that the use of biocides could lead to the development of antibiotic resistant bacteria has already been indicated by several laboratory studies. In practice it is so far very difficult to establish clearly and without a doubt whether using biocides leads to the emergence and proliferation of antibiotic resistant bacteria. There are no standard methods of testing for a link between the two, and the results from different laboratories are conflicting. More...
6.1 Biocides could pose a direct threat to human health if they lead to the survival of some harmful bacteria which are resistant to antimicrobial products. Even the emergence of harmless resistant bacteria as a result of biocide use could pose an indirect threat, since their genes that confer resistance might be transferred to harmful bacteria. More...
6.2 The improper use of disinfectants in intensive, industrial-scale farming could thus potentially lead indirectly to antibiotic-resistant infections in humans. More...

6.3 Bacteria resistant to biocides are increasingly common in health care settings. More research is needed to investigate whether there is a link between biocide use in hospitals and emergence of antibiotic resistance. To date, evidence of such a link has only been found in some cases of antibiotics that are not currently widely used.
Health care workers should be trained to use disinfectants and antiseptics properly and only when necessary. More...
6.4 Biocides are used in such large volumes that they can be found in small concentrations throughout the environment. There is a concern that continually exposing bacteria to biocide could lead to the emergence of resistant strains but this has not yet been clearly shown in practice. More...
7.1 Bacteria populations respond quickly to changing environments. When they are exposed to chemicals, such as biocides, that are toxic to them, resistance can emerge in different ways. Because biocides and antibiotics often work in a similar way, some of these resistance mechanisms are effective against both products. More...
7.2 Bacteria in homes and in the environment are likely to be repeatedly exposed to concentrations of biocides that are too low to kill them and this could lead to increased resistance. The actual spread, if any, of this problem is still unknown. More...
7.3 A bacterium can pass sections of DNA to another one. Each of these sections can contain several genes that may be beneficial to the bacterium receiving them, such as genes conferring the ability to alter or expel harmful substances. Exposing bacteria to biocides can lead to the survival of bacteria having resistance genes and resistance could spread as bacteria pass the genes to other bacteria. More...
7.4 Significant amounts of biocides reach kitchen sinks, wastewater treatment plants and surface waters. There is concern that these environmental concentrations might lead to resistance in micro-organisms but this was not confirmed by laboratory studies. More...
Antibiotic use is still the main cause of antibiotic resistance in clinical practice even if biocide use may play a role. To safeguard our ability to treat infections with antibiotics, a good hygiene to prevent infection and the appropriate use of biocides are crucial. More...
8.1 Different biocides act in different ways and some are more likely to lead to the emergence of resistant bacteria than others. The risk of spreading resistance genes depends on the type of bacteria involved, and is particularly high for bacteria that readily pass genetic information (DNA) to other types of bacteria.
Bacteria that grow as a biofilm attached to a surface are particularly able to survive hostile conditions (physical, chemical or biological attacks) and pose a high risk of resistance to both antibiotics and biocides. More...
8.2 It is very difficult to measure how effective antimicrobial products are, particularly in real life conditions.
There is an urgent need to develop standard testing methods of measuring both biocide and antibiotic resistance in bacterial samples, including bacteria that grow as a biofilm. More...
Humans have long used products with biocidal properties to effectively keep harmful micro-organisms at bay. Today, bacteria are becoming increasingly resistant to antibiotics and there is scientific evidence that the use and misuse of biocides such as disinfectants, antiseptics, or preservatives can contribute to antibiotic resistance. To date, the lack of precise data, in particular on quantities of biocides used, makes it impossible to determine which biocides create the highest risk of generating antibiotic resistance.
A clear assessment of the risk requires:
Biocides are a precious resource that should not be used unnecessarily. When they are used, they should be applied in concentrations high enough to kill all the bacteria exposed and eliminate the risk of resistance.

This summary is free and ad-free, as is all of our content. You can help us remain free and independant as well as to develop new ways to communicate science by becoming a Patron!