

Sprachen:

The effects of triclosan depend largely on the concentration used.
At high concentrations, triclosan works by interfering with the outer membrane that protects bacteria, making it permeable so that triclosan can penetrate it and kill the microorganism. At lower concentrations, triclosan attacks several targets. For instance, it slows down drastically several important biochemical reactions inside the bacteria.
Some bacteria have an innate resistance to triclosan, possibly because their outer membrane does not let it through. Bacteria can also become resistant to biocides using a variety of methods that lower the concentration of biocide inside the bacteria. For instance, some bacteria have mutated so that triclosan does not disrupt their vital biochemical reactions, or they have found ways of bypassing the steps in these reactions that are affected by triclosan. Other bacteria have developed systems that “pump out” any substances that are harmful to them, such as triclosan. In principle, some of these defence mechanisms can be passed not only from one generation of bacteria to the next, but also from one bacterium to another.
Different mechanisms may also work in conjunction and together, have a greater effect than each one has separately. For instance, some highly resistant bacteria have both: a modified outer membrane that does not let triclosan through easily, and ways of expelling any of the biocide that manages to get inside the cell.
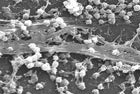
Biofilms require a special mention. Bacteria are rarely found as single individuals. Instead, huge numbers join together and attach themselves to surfaces forming a biofilm. These bacterial biofilms have a wide repertoire of defence mechanisms and are much more resistant to antimicrobials than are isolated bacteria. There is very little research in this field but there is some evidence that biocides could be ineffective against biofilms made of resistant bacteria. On a positive note, using triclosan followed by an antibiotic could be effective against bacterial biofilms. This would be extremely beneficial given the serious problems that biofilms pose in hospitals and other medical centres. More...
When bacteria are exposed to triclosan, some strains become resistant to it by mutating or by activating resistance genes. Some of these genes are also involved in cross-resistance and multi-resistance to different types of antibiotics and biocides so there is a concern that exposing bacteria to low concentrations of triclosan could lead to the emergence of highly resistant bacteria that would be very difficult or virtually impossible to eradicate. However, a study from 2004 found that treating bacteria with low concentrations of triclosan does not generally lead to drug-resistance, and any resistance cannot be transferred from one bacterial species to another.
Several laboratory studies have found that bacteria which are resistant to a biocide are also resistant to other types of antimicrobials. However, to date there is no evidence of a similar link in real situations outside the laboratory. The results vary with the concentration of biocide used and also with the species of microorganism investigated. Some bacteria that are treated with relatively low concentrations of triclosan become less susceptible to antibiotics. However, other types of bacteria are unaffected and, in the case of E. coli, triclosan-resistant bacteria were more easily treated with an antibiotic than the original or unexposed strain. More...
Triclosan is the most studied of all biocides but most of the research has been done on laboratory samples and at concentrations too low to be of relevance to real working situations. Despite these caveats, we can draw some useful conclusions.
A study from 2006 on bacteria collected from human saliva and a second one from 2004 on bacteria found in teeth concluded that repeated exposures to triclosan did not systematically produce high level triclosan resistance in all bacteria. A relatively small number of strains did become harder to treat to triclosan but many others didn’t. What is more, the increased resistance was limited to triclosan so even triclosan-resistant strains could still be killed by other biocides and by antibiotics.
A study from 2003 tested samples of bacteria collected in consumers’ homes and found that households that used antibacterial products had fewer harmful bacteria than those who didn’t. In both cases, the researchers did not find any evidence of cross resistance, and strains of bacteria that were resistant to antibiotics were still susceptible to antibacterial products. Users of antibacterial handwash did not harbour any more resistant strains of bacteria in their hands compared to non-users.
Triclosan is sometimes added to toothpaste to control plaque and improve the health of gums. These products are generally effective and there is no evidence that using triclosan-containing toothpaste leads to increased resistance or to cross-resistance.
With respect to microorganisms in the environment, whether or not a strain of bacteria becomes resistant to triclosan depends largely on the concentration of the substance that reaches it and this is by no means simple to measure. Triclosan attaches itself to solid particles and may bioaccumulate, posing a concern for aquatic organisms; but on the other hand, is degraded by ozone, chlorine, sunlight and by micro-organisms. Some of the concentrations of triclosan measured in the wastewater, sediments and sludge from wastewater treatment plants are high enough to affect microorganisms but we do not know how much of this triclosan is actually taken up by bacteria. In addition to triclosan, there are other biocides and antibiotics present in the environment and it is difficult to assess the effect of triclosan alone, or to understand how these different antimicrobials work when combined. More...
In most cases, resistance has been determined by measuring the minimum concentration of biocide that will stop bacterial growth (MIC). Whether or not a strain of bacteria is found to be resistant by this measure is largely irrelevant because the concentrations of triclosan used in practice are considerable larger than these MIC values, and are sufficient to kill all the bacteria treated, including those deemed to be resistant. For practical purposes, a better indicator of resistance is the minimum concentration that will kill the bacteria treated (MBC), which is closer to the real, in-use values.
Commercial products usually contain many ingredients in addition to triclosan, but laboratory studies usually dissolve triclosan in a single solvent. Therefore, it is difficult to make general conclusions since the effects of the biocide depend on the specific product involved and little is known about how different chemicals might act when combined.
There are studies which expose bacteria to low concentrations of a biocide and measure how bacterial growth changes with time. This is useful to determine changes in the characteristics of the bacteria that survive the biocide, but it does not tell whether or not bacteria will become resistant to the biocide and cross-resistant to unrelated compounds.
The methods used to determine antibiotic resistance are many and varied and this has lead to contradicting results. There are no standardised protocols that measure whether or not a biocide can lead to antibiotic-resistant bacteria, either because the bacteria become resistant or because the non-resistant bacteria are wiped out so that only the resistant or insusceptible strains survive.
It would be useful to develop tools to define the minimum concentration of a biocide that will select or trigger the emergence of a mechanism that will make bacteria antibiotic resistant. It would also be useful to link the specific genetic profile of bacteria with the resistance mechanism that they are likely to develop. Using modern genetic methods it may even be possible to develop routine tests that would identify bacteria with resistance mechanisms. More...

This summary is free and ad-free, as is all of our content. You can help us remain free and independant as well as to develop new ways to communicate science by becoming a Patron!